by Peter Buell Hirsch
Watch the full session of Conversations in Health: The Future of the Pharmacy and Pharmacist above.
The COVID-19 pandemic has shone a bright light on the critical role played by pharmacies, big and small, across America’s communities. Local pharmacies, in particular, have experienced a “back to the future” moment as they stepped up to help consumers across the country in traditional ways – serving as accessible sources of advice, comfort, education and guidance on everything from testing to vaccinations and other safety measures at work and in the home. At the same time, the powerful undercurrent of digitalization and virtualization of care has continued to transform the roles of the pharmacy and the pharmacist, opening up potential new avenues as others close.
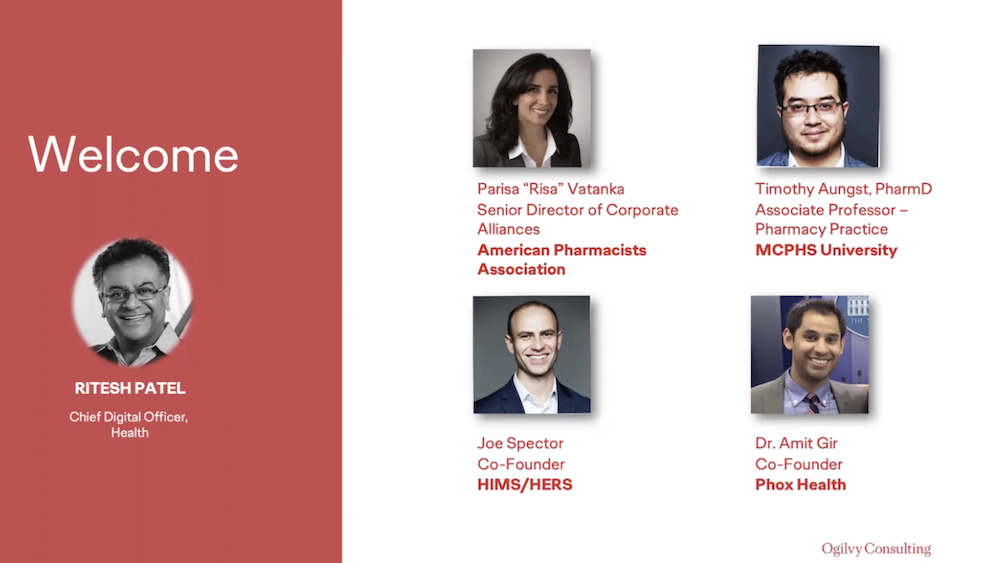
To discuss these themes and pharmacy-related opportunities and challenges in the evolving healthcare ecosystem, Ogilvy brought together four leaders in the pharmacy space -- Risa Vatanka, Senior Director, Corporate Alliances at the American Pharmacists Association; Timothy Aungst, Associate Professor of pharmacy practice at the Massachusetts College of Pharmacy and Health Sciences, with a focus on digital pharmacy; Joe Spector, co-founder of Hims & Hers, a telehealth company specializing in selling prescription and OTC products and personal care online; and Amit Gir, CEO and co-founder of Phox Health, which provides pharmacy delivery apps and services for health systems and telehealth companies, enabling prescriptions to be delivered to patients in two hours or less.
According to the panel, the future of pharmacy lies at the juncture of the digitalization and the consumerization (or democratization) of health, driven by a set of inter-related forces. Regardless of the specific outcome of this transformation, it seems improbable that the traditional model of pharmacy consisting of thousands of community sites, each staffed with highly trained and licensed pharmacists will persist for long. The growth of healthcare ecommerce as represented by Hims & Hers, as well as the third party just in time delivery model represented by Phox Health are clear evidence of this trend. As Tim Aungst suggested, the most likely development will be the emergence of a “hub and spoke” model, in which a smaller number of certified pharmacists validate prescriptions from centers of expertise, which are then filled by pharmacy technicians at community locations. In 10 years’ time, by his estimation, only 20-30% of pharmacies will have certified pharmacists on site.
According to Risa Vatanka, this is not the only change in the model that we should anticipate. In contrast to pharmacies in the rest of the world, American pharmacists are still spending huge amounts of time on manual pill processing: “our Achilles heel for decades has been this manual counting and repackaging of medications,” she says, not only wasting resources but creating medical errors. According to some estimates, non-optimized medication therapy costs the US $500 billion a year. These and other changes to the distribution and validation of medications, the panel agreed, raise profound questions not only about the future of community pharmacy but about the future of the profession itself. What happens, in their formulation, to the 10,000 – 20,000 pharmacists soon apparently to be left without a meaningful role?
To answer that question, Aungst suggests, we need to look at three parallel forces that are mutually reinforcing. The first is the transformation of care at the patient level. While most medications still come predominantly in pill form, an increasing number of therapies, especially those involving the treatment of chronic disease, take the form of infusion or injection therapies. Furthermore, many of these new therapies now come packaged with their own wireless administration and monitoring systems. The most innovative diabetes pumps which can now predict when a diabetic’s blood sugar level will change and administer insulin preemptively are only the most striking example of this confluence of drug and device.
At the same time, the slow but ineluctable drive towards value-based care is causing health systems to push patient care out of acute settings (the hospital) and into the patient’s home. Amit’s description of sending a mini-fridge containing medication to a patient’s home in time for a nurse practitioner’s visit is a telling example of this shift. This second of the three forces is only viable because of the emergence of wearable and mobile digital tracking devices by which providers can ensure, remotely, that their patients are in stable or improving health.
The third of the three forces is linked to the success of health businesses like Hims & Hers. As Joe Spector describes it, he and his partners identified the need to replace the cold, bureaucratic and even judgmental characteristics of so much retail health with a warmer, accepting, convenient patient experience, less akin to traditional healthcare practice and closer to the experiences that consumers are increasingly able to get from other interactions across the lifestyle space.
Paradoxically, the panel suggested, the confluences of these three forces is creating a role for the modern pharmacist that is at the same time highly traditional and entirely novel – to become the curator, translator and coach of the emerging data-mediated patient experience. Traditional, as the COVID-19 era has shown, in functioning as the patient’s always available counselor and guide; novel in the sense that the certified pharmacist is better positioned than any other professional to help set up, manage and interpret the increasing numbers of medications with digital companions. “Just give us the data,” as Aungst put it. He argued that the idea that doctors would have the time to devote to this type of long term real-time monitoring of their patients in this fashion is a fantasy not supported by the economics of patient care. Pharmacists are the ones, says Risa Vatanka, best positioned to “help determine when a patient is a candidate for a medication with a digital companion, help set up the device, monitor the patient on the portal, going from episodic to continuous care and communicating back and forth between the provider and the patient.”
While there are some regulatory hurdles to creating the “provider status” required to make this transition possible, perhaps the biggest obstacle, according to the panel, is economic. This shift will require a service model approach rather than the current commerce model by which pharmacies are paid by volume of prescriptions filled. According to Aungst, pharmacy has sufficient outcomes data demonstrating the clinical benefits of the role that pharmacists can play. What is currently lacking is the financial outcomes data needed to persuade payers that service style reimbursement of pharmacists will deliver successfully to the healthcare bottom line. But Vatanka is unperturbed by these challenges. As she put it, pharmacists can and should be the “Genius Bar” of consumer health.
Peter Buell Hirsch is an Adjunct Professor based at Department of Communication Studies, Baruch College, New York, New York, USA and Global Consulting Partner for Reputation & Risk Lead at Ogilvy Consulting.